About Age-Related Macular Degeneration
Macular degeneration is a term which includes hundreds of conditions affecting the macula. In this section we will be discussing age-related macular degeneration (AMD) also known as age-related maculopathy. AMD is the leading cause of blindness in adults over 55 years of age in the United States. The macula is the part of the retina responsible for central vision. This detailed vision is important for reading, watching TV and driving as well as any task requiring fine vision. The macula is the part of the retina most affected by macular degeneration.
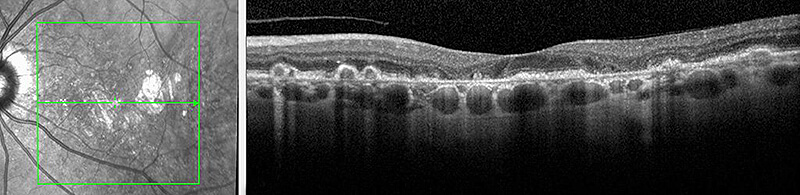
The retina is made up of several layers which line the inner wall of the eye. Each layer has a specific function and all work together to create vision. When light enters the eye it is focused by the cornea and lens onto the macula. The light is then converted into electrical signals by cells in the retina called photoreceptors. These photoreceptors send signals to the brain via the optic nerve which are then interpreted by the vision centers in the brain. In AMD, these cells or photoreceptors break down over time and eventually accumulate under the retina. These accumulations appear as yellow deposits called drusen. It is believed that drusen and associated waste products prevent adequate nutrition from reaching the retinal cells. The characteristics of these drusen and the amount of damage to the macula are used to determine the severity of AMD. Usually, as the number and size of drusen increases, the severity of AMD increases and visual symptoms worsen.
AMD is divided into two general categories, dry AMD (DAMD) and wet AMD (WAMD). A simple way to think about these two categories is that in WAMD there are abnormal blood vessels growing under or in the retina which may leak blood and fluid, while in DAMD there are no abnormally growing blood vessels. Dry AMD often results in a gradual loss of vision while wet AMD may result in a sudden and sometimes more severe loss of vision.
Dry Macular Degeneration (DAMD)
Approximately 90% of patients with AMD have the dry form. Dry macular degeneration is often divided into three stages – early, intermediate and advanced. Early stage DAMD begins with the formation of small drusen. There may not be any loss of vision at this stage. However, as more drusen develop and become larger (intermediate DAMD) the central vision may slowly become blurry, dim or faded. In advanced DAMD the build up of drusen eventually causes associated retinal cells to die. The process of cell death is called atrophy. If the disease progresses these areas of atrophy can become larger and more dense, causing further damage to the macula. Over time this can result in a significant decrease in central vision.
Wet Macular Degeneration (WAMD)
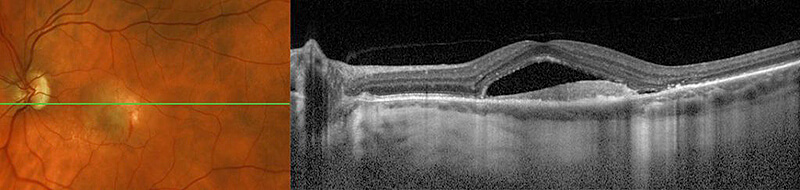
Approximately 10% of patients with AMD have the wet form. Patients with wet AMD start out with the dry form of AMD initially. In WAMD, abnormal blood vessels start growing within or underneath the retina from a layer called the choroid. The growth of these abnormal blood vessels is called choroidal neovascularization (CNV) and can lead to the leakage of fluid and blood which defines WAMD. With the pooling of fluid and blood underneath the photoreceptor layer (the layer responsible for transmitting signals to the brain) the retina is no longer able to function normally which often causes a sudden change in vision. The abnormal blood vessels and bleeding can also cause further scarring (fibrosis) of the retina. Scarring from WAMD in the macula may cause an irreversible loss of central vision.
Symptoms vary in type and severity from patient to patient and between dry and wet AMD. Typically however, dry AMD patients may notice a blurred area or spot in their central vision. The blurred area or spot may vary in shade from grey to black. Some patients notice dim, faded or blank areas. Over time these symptoms may worsen and affect central vision to a point where reading, driving and other daily tasks may become difficult. Wet AMD patients may have an additional symptom of distortion, whereby straight lines appear wavy or crooked. For example, a door frame, venetian blinds or floor tiles appear bent or warped. Visual distortion can indicate the development of abnormal blood vessels. The quicker these abnormal blood vessels are treated, the better the visual prognosis. Therefore, it is important with wet or dry AMD to monitor each eye closely.
To monitor for changes in visual symptoms, an Amsler grid is recommended. The Amsler grid will help with monitoring one eye at a time which is the best way to determine if any change is occurring in either eye. It is also helpful to monitor vision by closing one eye at a time while performing activities that require detailed vision such as watching TV, reading, driving etc. The goal is to get accustomed to the vision of each eye independently to enable a comparison of the vision in each eye from one day to the next. This allows for easier detection of subtle changes in vision in either eye which may occur very gradually.

If new symptoms or visual distortion is discovered, it is important to be evaluated without delay. In addition to a dilated eye exam, tests may be performed to determine if wet AMD is present. An OCT (optical coherence tomography) scan will be obtained to check for signs of leakage or fluid building up under the macula. A fluorescein angiogram (FA) can also help detect the presence or location of active WAMD or CNV. During the FA, a diluted synthetic dye is injected into an arm vein and pictures are taken which illuminate the flow of the blood vessels in the retina. If abnormal blood vessels are growing due to wet AMD the dye will begin to leak from these areas.
While we do not know the exact cause of AMD, it usually occurs in adults fifty years of age or older. It is theorized that years of damage from UV light as well as blood flow alterations and inflammation may lead to or worsen AMD. Certain studies indicate that cardiovascular disease and high lipid levels may also contribute to the formation or worsening of AMD. Still it is not yet clear whether these factors are merely associated with or actually cause AMD.
Although we do not know the precise cause of macular degeneration, we do know there are specific risk factors which increase the likelihood of developing AMD.
-
Age – AMD incidence increases with age.
-
Genetics – we do know that genetics plays an important role in the development of many diseases including AMD. If there is a family history of AMD then the chance of developing the condition is higher. Certain populations have a higher incidence of AMD than others. For instance, Caucasians have a higher risk of advanced AMD. Many studies are being performed to further understand the genetics of AMD. If you are diagnosed with AMD it is a good idea for your children to have a yearly examination by their eye doctor especially as they get older.
-
Smoking – Studies show that smokers have between a two to seven times higher risk of developing AMD as compared to non-smokers. In addition there is up to a five times greater chance for severe vision loss from macular degeneration in smokers.
-
High blood pressure and cardiovascular disease – We also know that high blood pressure and cardiovascular disease are associated with AMD.
-
Obesity – Body mass index (BMI) is a measurement comparing weight relative to height. An increased BMI is associated with AMD. Also, central obesity (weight around your middle) is a higher risk than that of general distributed obesity. In other words, increased weight around the middle is associated with AMD.
-
Inflammation – Research has shown that AMD is associated with inflammation. Although inflammation is a normal part of our immune system, evidence indicates abnormal ocular inflammation may play a role in AMD.
-
Sunlight exposure – most experts agree there is a relationship between heavy sunlight exposure and the development of AMD. We do not know whether sunlight exposure at a young age versus an older age is more damaging. Therefore, patients with AMD and their family members are urged to protect their eyes from sunlight with UV light blocking sunglasses. Check your sunglasses to be sure that they protect against 100% of UVA and UVB light.
For many years, there were no available treatment options for patients with the dry form of macular degeneration, other than vitamin supplements that the Age-Related Eye Disease Study (AREDS) demonstrated could slow progression. As of August 4, 2023, there are now two medications approved by the U.S. Food and Drug Administration (FDA) to treat the most advanced form of dry macular degeneration called geographic atrophy (GA). Both treatment options, pegcetacoplan (Syfovre) and avacincaptad pegal (Izervay), are delivered every 25-60 days, depending on the need of the specific patient, and have been shown to slow the progression of geographic atrophy.
The Age-Related Eye Disease Study (AREDS) proved that a specific combination of nutritional and vitamin supplements can slow down the progression of AMD and help preserve vision. The subsequent AREDS2 trial made some additional comparisons and the recommendations from the the AREDS2 trial is as follows:
- Vitamin C 500mg
- Vitamin E 400 international units
- Zinc oxide 80mg
- Copper 2mg
- Lutein 10mg and zeaxanthin 2mg
The AREDS study also showed the value of eating a diet rich in green, leafy vegetables, fruits, berries, and fish a few times per week. It is important to discuss your nutritional supplements with your primary care physician.
For some, a low-vision specialist can train patients in the use of optical devices and equipment that can help maximize vision potential as well share information about support groups and other available resources. Often a referral to a Low Vision Specialist can be very helpful in showing patients with significant visual loss how to perform their daily activities such as reading, watching television, or getting around independently.
Treatment of Wet AMD
Wet AMD occurs when abnormal blood vessels grow within or underneath the retina. They usually grow from the choroid layer which lies under the retina but they can also occur from the retina as well.
There are numerous treatments available for these abnormally growing and leaking blood vessels including: intravitreal injections, thermal laser, photodynamic therapy (PDT) or a combination of these treatments.
For additional information, please visit the ASRS page on age-related macular degeneration.
For additional information please visit the National Eye Institute page on macular degeneration or the ASRS page on macular degeneration.

