About Diabetic Retinopathy
Diabetic retinopathy is a leading cause of blindness in adults in the United States. A large percentage of diabetics develop this progressive eye disease, even when blood sugar levels are well controlled. The longer a patient has diabetes, the greater the chances are of developing eye problems. Additionally, the severity of diabetic retinopathy is thought to be related to high or inconsistent glucose levels as well as elevated blood pressure. The hemoglobin A1C is a blood test that estimates an average glucose level over several months prior to the blood test being drawn. This gives a more accurate measure of how well the disease is being controlled. It is important to have A1C scores, blood sugar levels, and blood pressure monitored by a primary care physician or endocrinologist. Diabetic retinopathy is usually divided into two groups: background diabetic retinopathy (BDR) and proliferative diabetic retinopathy (PDR).
Background Diabetic Retinopathy (BDR)
In BDR, the blood vessels of the retina become weak and fragile from the underlying systemic diabetes. The damaged blood vessels have weakened walls and can develop microscopic bulges called microaneurysms. Blood or blood products can leak through the walls of the vessels or capillaries causing retinal hemorrhages and possibly retinal swelling (edema). Vision can remain unchanged with early diabetic changes. However, if this leakage results in an accumulation of fluid and blood in the retina, then a decline in vision can occur. These clinical findings can be found in the peripheral retina as well as the central retina or macula. With macular edema, vision can worsen, become blurred, dark or distorted. BDR can be rated in severity: from mild, moderate or severe.
Proliferative Diabetic Retinopathy (PDR)
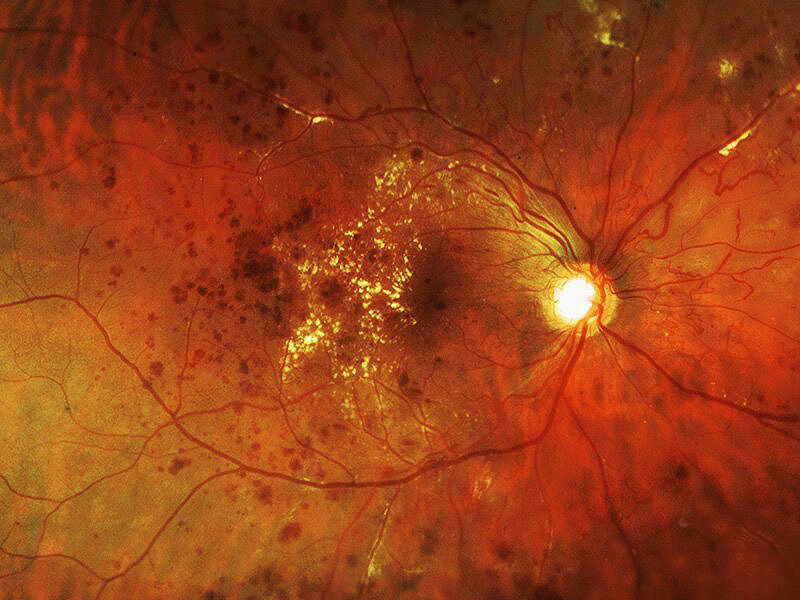
As BDR becomes more severe, further obstruction of the retinal blood vessels results in a loss of circulation (ischemia), and the formation of abnormal blood vessels (neovascularization) in the peripheral retina. Ischemia and neovascularization are the first signs of PDR. The longer the retina has gone without adequate blood flow, the more severe the diabetic retinopathy. Portions of the retina that become ischemic will eventually lose the ability to function properly. If ischemia occurs in the macula, permanent loss of central vision can occur.
As PDR becomes more severe, abnormal blood vessels may begin to grow into the vitreous gel as well as on the surface of the retina and other eye structures. Neovascularization of the optic disc (NVD) and neovascularization elsewhere on the retina (NVE) can occur in addition to neovascularization of the iris (NVI). NVI is a condition that may lead to high pressure in the eye (neovascular glaucoma) which can cause severe pain and permanent loss of vision.
Abnormal blood vessels caused by PDR are fragile and often break, causing vitreous hemorrhage or bleeding inside the eye. This can cause a sudden decrease in vision often accompanied by floating spots or cobwebs. Neovascularization from PDR can also lead to scar tissue formation and traction or pulling on the retina. A traction retinal detachment (TRD) is a serious complication which, if left untreated, could result in complete blindness.
Diagnosis and Testing
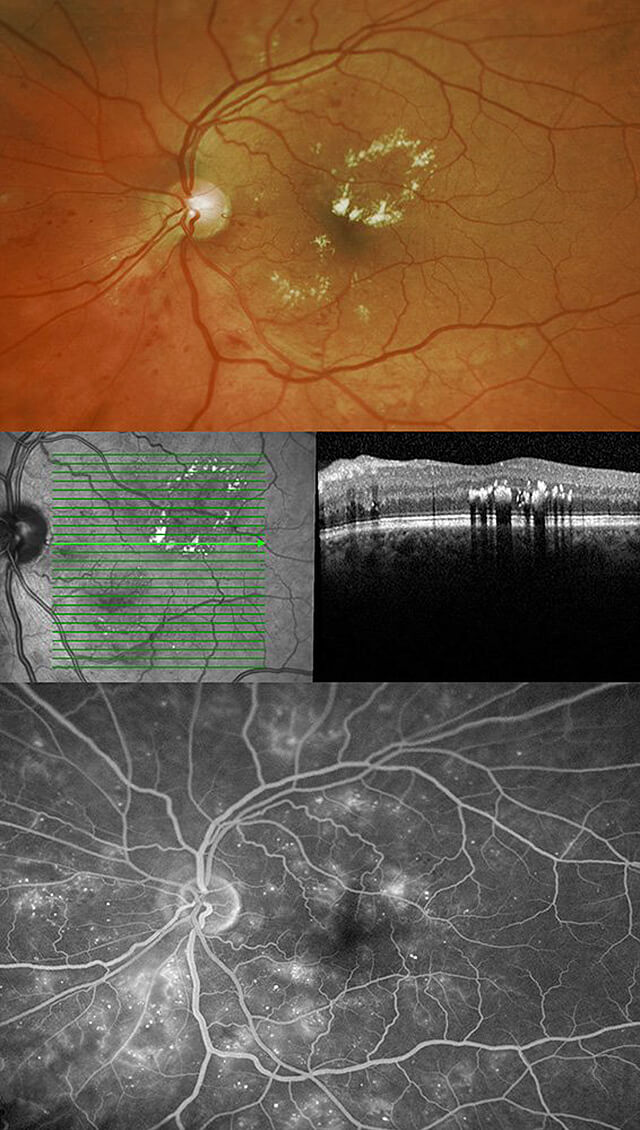
A dilated eye examination is required to fully determine if there are any signs of diabetic retinopathy. The risk of BDR and PDR increases with the amount of time since the initial diagnosis of diabetes. After 15 years, most diabetics will have some signs of diabetic retinopathy. Optical coherence tomography (OCT), fluorescein angiography (FA), and fundus photographs (FP) are tests which may be ordered to aid in diagnosing diabetic retinopathy and monitoring for changes. OPTOS panoramic photography is the very latest technology which can provide a wide-field, 360 degree view of the retina. If vitreous hemorrhage is present, blocking the view of the retina, an ultrasound exam may be performed which can scan internal eye structures and display any abnormal findings.
Treatment
The newest treatments for diabetic retinopathy involve the use of medications which can be effective not only in stabilizing diabetic retinopathy but also in restoring vision in many cases. These medications are injected into the eye through an office-based procedure called an intravitreal injection. This relatively painless injection, through the white part of the eye, is performed after the eye is thoroughly anesthetized with topical eye drops. Drugs such as Eylea, Lucentis and Avastin have the potential to improve vision by reducing the amount of macular edema caused by diabetic retinopathy. Steroids such as Triescence and Kenalog have also been successful in reducing diabetic macular edema. Often a combination of laser therapy and injectable medication is used. Although complications and side effects are rare with intravitreal injections they include ineffective treatment, bleeding, infection, inflammation, cataract formation, retinal detachment, glaucoma and loss of vision.
Laser therapy or photocoagulation, has been proven effective in controlling BDR and PDR in the majority of patients. The primary goal of laser therapy is to prevent further visual loss. For clinically significant macular edema, the laser is focused in the macula (focal or grid therapy) in order to reduce the leakage of the retinal blood vessels which threatens the central vision. In PDR, laser is used to treat the areas of peripheral retina with poor circulation or ischemia. This form of laser is called pan-retinal photocoagulation (PRP). The purpose of PRP treatment is to decrease abnormal blood vessel growth and decrease the risk of additional complications from PDR. It can take days, weeks, or months for the laser to reach its maximal effect. In most cases of PDR, the visual prognosis is better the earlier it is detected and treatment is initiated. Although risks with laser treatments are minimal they include ineffective treatment, bleeding, increased edema, cataract and loss of vision.
Because diabetes is a chronic condition, diabetic retinopathy may continue to worsen over time, requiring additional laser treatments, injections or possibly retinal surgery. If a vitreous hemorrhage does not clear spontaneously or if a build-up of scar tissue creates traction on the surface of the retina, vitreous surgery may be required to remove the hemorrhage and scar tissue in order to stabilize the retina and maximize vision. Risks of surgery can include ineffective treatment, infection, additional bleeding, the need for further surgery, worsening vision, or cataract progression in those patients who have not undergone cataract surgery. With each surgical case the retinal surgeon will discuss all available treatment options along with their potential benefits and risks.
For additional information, please visit the ASRS page on diabetic retinopathy.