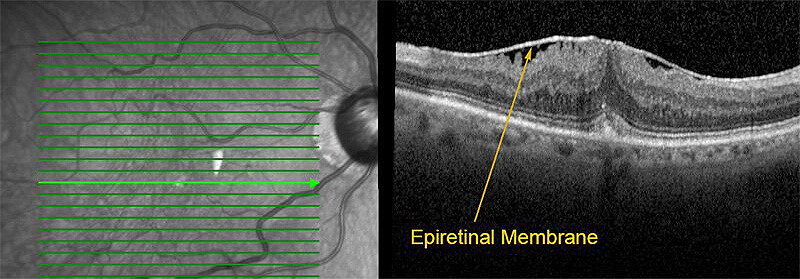
About Epiretinal Membrane
Epiretinal membranes can develop as a result of natural changes in the eye and vitreous gel due to aging, or they can be secondary to prior eye surgery, history of retinal detachment, trauma, blood vessel abnormalities, or inflammation. Diagnosis of epiretinal membranes is typically made through a combination of the dilated examination, optical coherence tomography (OCT), and sometimes fluorescein angiography.
Not all epiretinal membranes require treatment. If they are mild and do not cause visual symptoms, they can be observed. If they cause blurred or distorted vision, they can be treated with vitrectomy surgery. Vitrectomy surgery is typically performed on an outpatient basis. During the procedure, the surgeon removes the vitreous gel (which is replaced with a sterile saline solution), and carefully peels away the epiretinal membrane. The most common risk of the surgery is an increase in the risk of cataract formation. Less common risks include the risk of retinal tear or retinal detachment, serious infection, or regrowth of the epiretinal membrane. Visual improvement tends to be gradual and occurs over the course of several months. The amount of visual improvement depends upon the severity and duration of the epiretinal membrane and the presence of other eye problems.
For additional information, please visit the ASRS page on epiretinal membrane.