About Macular Hole
The retina is the delicate, light-sensitive nerve tissue which lines the inside of the eye and is responsible for vision. The macula is the central portion of the retina and is responsible for “straight ahead” vision, as well as a portion of the peripheral vision. The macula is composed of several layers, each having a specific function, and is normally smooth and flat against the back wall of the eye. Within the central macula lies the fovea, an area about the size of the head of a pin, which is responsible for fine or detailed vision such as is required in reading, writing, and driving. Injury or disease within this area, such as a macular hole, can lead to a dramatic loss of vision and significant visual impairment. While their exact cause is unknown, macular holes have been associated with several eye disorders including diabetic retinopathy, near-sightedness (myopia), Best’s disease, and ocular trauma. The most common cause may be related to aging.
As a result of the normal aging process, the gel-like vitreous which fills the inside cavity of the eye, condenses over time and changes in consistency and shape. As it condenses, the vitreous collapses and separates from the retinal surface, usually without consequence. However, it is felt that in some cases, the vitreous is unusually adherent to the retina and creates a condition called vitreomacular traction (VMT). Traction on the surface of the macula can lead to the formation of a macular hole.
Symptoms and Diagnosis

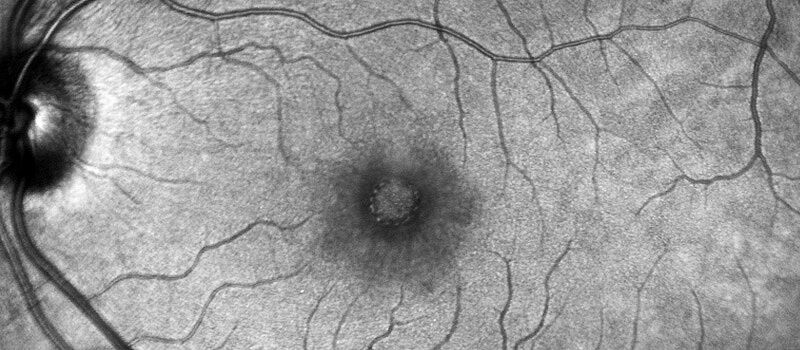
Macular hole symptoms are varied but usually involve a change in vision such as a blank area, dark spot, or area of distortion in the central vision. These changes may happen gradually or quite suddenly. A dilated eye exam is usually required to accurately diagnose a macular hole. Diagnostic testing is also performed to confirm the diagnosis as well as to provide additional information about the characteristics of the macular hole. Since macular holes vary in cause, thickness and severity, an Optical Coherence Tomography (OCT) test can provide a cross sectional image of the macula which documents the subtle characteristics of the macular hole. This information may be helpful in determining the best course of treatment. A fluorescein angiogram (FA) is a photographic test which uses a special contrast dye to evaluate the retinal circulation and may also be recommended if additional diagnoses or underlying conditions are suspected.
Treatment
An out-patient surgical procedure called a trans pars plana vitrectomy (TPPV) is usually required to repair a macular hole. During a vitrectomy, the gel-like vitreous is removed from the eye and replaced with a saline solution. Any membranes or residual vitreous which may be causing traction on the retinal surface are carefully removed using micro- scissors and forceps. Removing the source of the traction greatly assists in the closure of the macular hole. A bubble of a special gas and air mixture is then used to replace the saline in the vitreous cavity. The surface tension created by the bubble flattens and smoothes the retinal surface and closes the macular hole. Placing the bubble precisely over the macula following surgery is essential to ensure closure of the macular hole as the eye heals. This is achieved by maintaining a face-down position for several days after surgery. The bubble is eventually absorbed and replaced naturally by the aqueous humor, the fluid in the front chamber of the eye.
Outcome and Expectations
The visual prognosis after macular hole surgery is good in most cases. The size, severity, and location of the macular hole as well as the duration often dictate the visual potential after surgery. A macular hole with a duration greater than six months will typically not have as good a visual prognosis as a recent onset macular hole. The goal of surgery is to improve the central vision and lessen any visual symptoms present before surgery such as blank areas, blurriness and distortion.
As with any surgical procedure there are potential benefits and risks which will be discussed by the physician prior to surgery. With respect to macular holes, there is a small chance the hole will re-open which could require additional surgery. In addition, there is about a ten percent chance the fellow-eye will develop a macular hole over time.
For additional information, please visit the ASRS page on macular hole.

