About PVD, Retinal Holes, Tears or Detachments
The retina is composed of several thin layers of light-sensitive nerve cells that line the back of the eye. When an image is focused onto the surface of the retina, a signal is sent to the visual cortex of the brain via the optic nerve and vision is produced. Different parts of the retina contribute to different parts of vision. The center of the retina, or macula, allows for fine, detailed, central vision while the area of retina surrounding the macula is referred to as the peripheral retina and is responsible for side, or peripheral vision. The central cavity of the eye is filled with a clear, gel-like fluid called vitreous humor which is adherent to the retina, blood vessels and optic nerve. Changes to the retina and vitreous humor due to eye disease, ocular trauma or even the normal aging process can lead to posterior vitreous detachment (PVD) , peripheral retinal holes or tears, or more seriously, retinal detachment (RD).
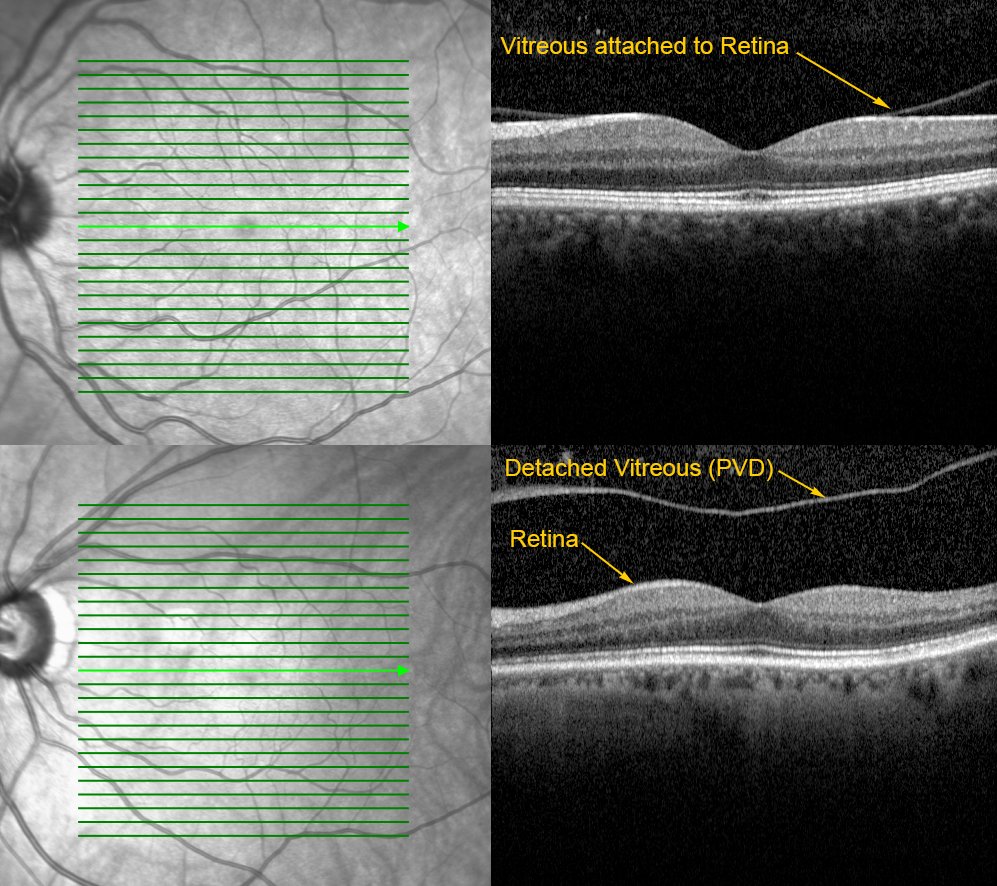
Posterior Vitreous Detachment
Due to the normal aging process or other factors, the vitreous humor may condense or shrink over time causing a separation of the vitreous from the surface of the retina. This fairly common condition is called a posterior vitreous detachment or PVD. As the vitreous becomes more liquid, pigment cells, blood cells, or other vitreous debris may become more mobile, causing floating spots, shadows or cobwebs to appear in the vision. Additionally, if the vitreous is adherent to the retinal surface as it begins to condense, any tugging or pulling on the retinal surface may cause bright flashes of light or sparks to appear in the vision. These symptoms of “flashes” and “floaters” may temporarily obscure vision and become quite bothersome but usually subside over time. Though posterior vitreous detachments rarely require treatment, a dilated eye exam is required as soon as possible to rule out the possibility the retina has developed a peripheral retinal hole or tear during the PVD process, as the symptoms may be the same.
Peripheral Retinal Holes and Tears
Peripheral retinal holes and tears are defects in the retina which may be caused by a number of conditions including PVD, retinal traction, ocular trauma and high myopia (nearsightedness). This is usually an urgent condition requiring treatment as soon as possible. Though common symptoms include a sudden onset of flashes and floaters, peripheral retinal holes and tears may present with no visual symptoms at all. However, if left untreated, peripheral retinal holes and tears may lead to a retinal detachment by allowing fluid from the vitreous cavity to collect underneath the retina. Peripheral retinal holes and tears are typically treated with office-based procedures such as laser therapy or a procedure using a frozen probe (cryoretinopexy). These procedures can treat retinal holes and tears by creating adhesions which attach the retina to the underlying layers, thus preventing a retinal detachment. Risks and complications associated with these procedures are rare but include ineffective treatment, inflammation, bleeding, pain and cataract formation.
Retinal Detachment
A retinal detachment (RD) is a serious eye condition in which the retina has separated from the underlying layers of the eye. As fluid from the vitreous collects under the retina the light sensitive cells (photoreceptors) cease to function properly, causing a loss of vision wherever the retina is detached. This is usually an urgent condition requiring treatment as soon as possible. If left untreated, a retinal detachment could lead to a permanent loss of vision or even complete blindness. Common causes include retinal holes or tears, ocular trauma, high myopia, retinal scarring and traction, or other eye diseases. In addition to a sudden onset of flashes and floaters, other symptoms may include a sudden loss of central vision or a persistent, dark curtain or shadow which obscures a portion or all of the vision. Depending on several factors including size, location, duration and cause of the retinal detachment, surgical intervention is most often required to repair a detached retina.
Retinal Detachment Repair
Most retinal detachments are caused by retinal holes or tears which allow fluid from the vitreous cavity to collect under the retina. A trans pars plana vitrectomy or TPPV is a hospital-based, out-patient surgical procedure used to repair a detached retina by removing the gel-like vitreous and replacing it with a saline solution. Using a microscope and specialized instruments, the retinal surgeon removes the vitreous which relieves any retinal traction or pulling that may be caused by vitreous adhesions on the retinal surface. During a vitrectomy, fluid may also be drained from underneath the retina while air or gas mixtures are used in the eye to flatten or re-attach the retina. Once the retina is re-attached a laser can be used to seal the holes or tears which caused the detachment. Additional procedures may be performed in conjunction with a vitrectomy depending on the cause or complexity of the retinal detachment.
An elastic silicone band or scleral buckle (SB) is often used to encircle the eye during retinal detachment surgery. The scleral buckle creates an indentation in the outer wall of the eye (sclera) in order to provide support to the retina and to relieve any traction on the retinal surface. Scleral buckles, bands and sponges are used to help flatten and re-attach the retina during surgery and are usually implanted permanently. Since scleral buckles are covered by the conjunctiva (the skin that covers the sclera), they are usually comfortable and do not typically change the outward appearance of the eye.
As mentioned before, air bubbles and special gas mixtures are also used in the eye to help re-attach the retina. Bubbles of air and gas help to smooth and flatten the retinal surface during retinal detachment surgery and essentially “float” the retina back into position. Additionally, patients are often required to maintain a face-down position for several days following surgery as the special air and gas mixtures help to ensure retinal re-attachment as the eye heals. Air and gas mixtures are temporary and are eventually absorbed and replaced naturally by the aqueous humor, the fluid which fills the front chamber of the eye. While most often used during hospital-based surgery, air and gas mixtures can also be used in the office to repair smaller and less complex retinal detachments. In office-based pneumatic retinopexy procedures, special gas mixtures are injected in the eye in order to re-attach the retina. The patient is sent home with instructions to maintain a certain head position in order to carefully position the gas bubble. Once the retina is re-attached a laser or freezing probe can be used to seal any retinal holes or tears and essentially “tack” the retina into position.
If scar tissue membranes are present, a membrane peeling procedure is indicated during retinal surgery. Scar tissue on the surface of the retina may contract, creating retinal tears, folds and wrinkles. Micro-scissors, picks and forceps are used to release any traction caused by scar tissue which may be preventing the retina from re-attaching.
In complex retinal detachment cases involving excessive traction and scar tissue, silicone oil may be used to replace the vitreous during surgery in order to provide a long-term barrier against re-detachment. Silicone oil is typically removed once the re-attached retina has healed and become more stable.
Risks, Benefits, Complications, Side Effects and Expectations
As with any surgical procedure there are possible risks and benefits. Though unlikely to occur, the associated risks, complications and side effects will be discussed in detail before scheduling any surgical procedure. Based upon each individual case, the potential benefits as well as what to expect before, during and after each surgical procedure will also be discussed prior to scheduling surgery.
For additional information, please visit the ASRS pages on posterior vitreous detachment, retinal tears and retinal detachment.

