About Uveitis
Uveitis is an umbrella term meaning inflammation of the eye. Uveitis can damage vital eye tissue, leading to permanent vision loss. One way to categorize uveitis is based on which part of the uvea is affected.
Inflammation near the front of the eye is called anterior uveitis. Often, patients experience red eye, light sensitivity, and eye pain. It can start suddenly and symptoms can last up for weeks. Some forms of anterior uveitis are ongoing, while others go away but keep coming back- we call this recurrent anterior uveitis.
Inflammation in the middle of the eye is called intermediate uveitis or pars planitis. Patients may experience floaters (black spots in your vision) and blurred vision. Symptoms can last for a few weeks to many years. This form can go through cycles of getting better, then getting worse.
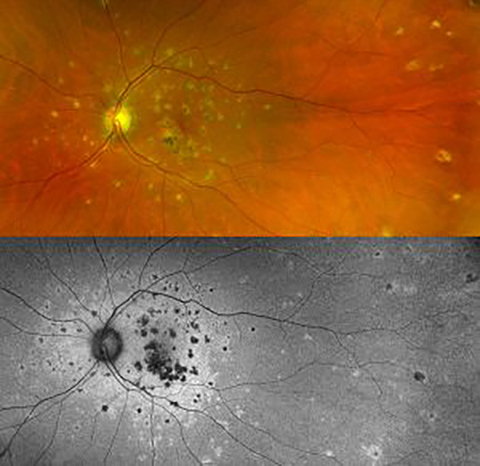
Inflammation toward the back of the eye is called posterior uveitis. Patients may experience blurred vision, distortion, floaters and color vision abnormalities. Symptoms can develop gradually and last for many years.
In severe cases, all layers may be involved and this is called panuveitis. Uveitis may affect one or both eyes, either at the same time or alternating.
If any of the above symptoms occur, it’s important to see a retina specialist immediately to have your eye(s) examined. Additional ancillary tests may also be conducted during your office visit to help better define the type and location of your eye inflammation. Even the most experienced eye physicians do not always know what causes uveitis.
However, since uveitis is often connected with other diseases or conditions such as infections or auto-immune diseases, some additional outside tests may be needed. They may include a physical exam, blood or skin tests, examination of eye fluids, and imaging tests.
Depending on the cause, uveitis is often treated with eye drop medicine that reduces inflammation (corticosteroids). Eye drops used to widen (dilate) the pupil may also be used which helps reduce pain and swelling. Sometimes medicine may need to be given by injection (shots) or taken by mouth.
Often times, your ophthalmologist will work with a rheumatologist, a specialized internal medicine physician with extra training in inflammatory disease, to help treat you. With this knowledge, we can work to employ the best treatment options available to minimize, if not cure, your eye disease and maximize visual outcomes.
For treatment of Uveitis in Austin, Texas, call 800-252-8259.
For additional information, please visit the ASRS page on uveitis.

